Paediatric ST8 Trainee
Royal Derby Hospital NHS Foundation Trust, United Kingdom
Title : Rising prevalence of Congenital Hyperinsulinism (CHI) in a neonatal unit: concern or coincidence?
Abstract:
Background: Hyperinsulinaemic hypoglycaemia (HH), the hallmark of congenital hyperinsulinism (CHI), is the most common cause of persistent hypoketotic hypoglycaemia in neonates and infants and carries a high risk of permanent brain injury if not promptly treated. Early diagnosis and management are essential to prevent features of irreversible brain damage viz epilepsy, cerebral palsy, and neurodevelopmental impairment1. Following birth, healthy neonates experience a transient fall in plasma glucose, which normally stabilises by 48 hours through adequate substrate availability and intact endocrine regulation of glucose homeostasis.2,3
In neonates with recurrent or persistent hypoglycaemia, CHI should be suspected. A plasma glucose <3 mmol/L, requiring a glucose infusion rate >8 mg/kg/min to maintain euglycaemia is highly suggestive.1 Biochemically, CHI is characterised by inappropriate insulin and C-peptide secretion during hypoglycaemia, with suppressed ketone bodies and free fatty acids (FFA).1,2
Early diagnosis and standardised management are critical to prevent long-term morbidity. A recent increase in CHI cases was observed in our neonatal unit.
Aim: To determine the causes of CHI in our centre and identify factors contributing to observed rise in prevalence.
Methods: This combined retrospective and prospective study evaluated neonates with hypoglycaemia and biochemical evidence of hyperinsulinism admitted to our unit. Management was benchmarked against national quaternary CHI centres. The study was prompted by a marked increase in CHI cases over a 12-month period (October 2024 – September 2025).
Results: A marked increase in CHI cases was observed over a 12-month period compared with the preceding two years. A term-to-preterm ratio of 1:4 was observed, with no sex or racial predilection. Antenatal risk factors for hyperinsulinaemic hypoglycaemia were identified in 30% of cases, including intrauterine growth restriction, maternal pregnancy-induced or chronic hypertension (notably beta-blocker use), and gestational diabetes. All infants demonstrated elevated serum insulin levels (>2 mU/L), ranging from 54.2 to 5802 mU/L (mean 916.1 ± 814.4), and raised C-peptide levels (541–2989; mean 1346.4 ± 367.3). The mean glucose infusion rate required to maintain euglycaemia was 13.49 ± 0.9 mg/kg/min, with all infants recording plasma glucose <3 mmol/L. Free fatty acid levels were available in six infants, and β-hydroxybutyrate levels were ≤0.1 mmol/L in all, indicating suppressed ketogenesis. All infants required increased glucose concentration delivery and high-calorie feeds/volumes to maintain euglycemia. Diazoxide therapy was required in 50% at discharge, with two infants failing glucagon trials prior. Of the 50% diazoxide responsive, the genetic subtype of CHI remains unknown. All infants successfully completed a six-hour fast before discharge.
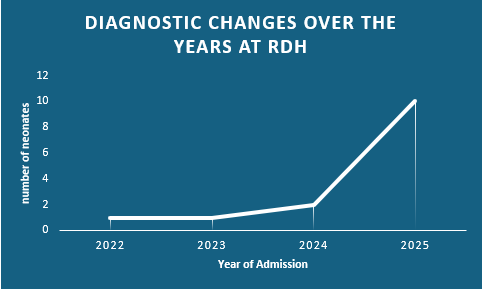
Conclusion: A significant increase in CHI cases was observed, predominantly among term infants. Early recognition, prompt biochemical evaluation, and standardised management pathways are essential to minimise neurological morbidity. Further work is needed to explore underlying genetic and population-level contributors to this rising prevalence.
Biography:
Dr. Osayuwamen (Yuwa) Egharevba is a Paediatric ST8 trainee undertaking Specialist Interest (SPIN) training in Neonatology in the East Midlands, England. She holds an MBBS from the University of Benin, Nigeria, is a Fellow of the West African College of Physicians (FWACP, Paediatrics), and a Member of the Royal College of Paediatrics and Child Health (MRCPCH). She holds a Postgraduate Certificate in Medical Education and has several academic publications to her name. She has worked as a paediatrician in a Nigerian teaching hospital and currently practises in the UK, with interests in neonatology, medical education, and global child health.
Copyright 2024 Mathews International LLC All Rights Reserved